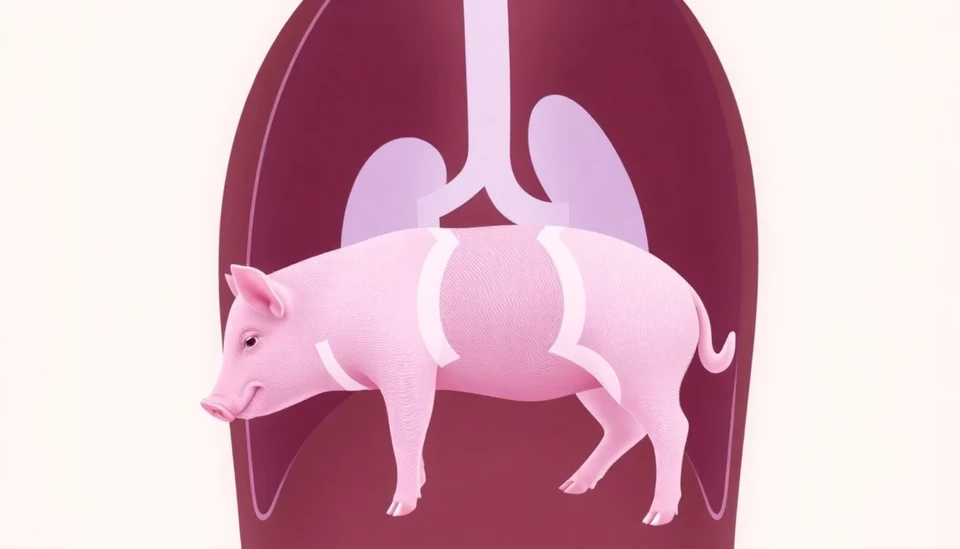
The Food and Drug Administration (FDA) has taken a significant step toward addressing organ shortages by greenlighting clinical studies that explore the possibility of transplanting pig kidneys into human patients. This decision marks a pivotal moment in xenotransplantation, wherein organs from genetically modified animals could be used to save lives and alleviate the currently overwhelming demand for human organ transplants.
Xenotransplantation, as it is known, has been a topic of debate and experimentation for decades, particularly as the number of individuals awaiting organ donations continues to rise. The FDA's recent approval allows researchers to initiate clinical trials that will evaluate the safety and efficacy of transplanting kidneys from specially bred pigs into humans, potentially revolutionizing the field of organ transplantation.
According to the United Network for Organ Sharing, there are currently over 100,000 people on the waiting list for kidney transplants in the United States alone. The annual number of kidney donations does not meet this urgent need, creating a dire situation for patients suffering from end-stage renal disease. The FDA's endorsement of these studies could pave the way for advancements that significantly bridge this gap.
The trials are expected to begin with closely monitored procedures to assess how the human immune system interacts with the pig kidneys. Researchers will closely observe potential rejection responses as well as any other complications that may arise from the transplant process. Through this careful study, scientists hope to gather valuable data that will not only inform future operations but also enhance our understanding of bioethical and safety considerations linked to xenotransplantation.
These pig kidneys are genetically engineered to reduce the risk of rejection and other adverse reactions, a critical factor that has hampered past attempts at cross-species organ transplants. This innovative approach reflects advancements in genetic engineering technologies, particularly CRISPR, which has made it possible to modify genes with unprecedented precision.
If trials prove successful, the implications for patients, families, and the broader healthcare community could be profound. Beyond providing new sources of organs, such innovations could lessen waiting times and the anxiety that comes with needing a transplant. They could also represent a significant shift in medical practices, ideally leading to a future where organ shortages are a concern of the past.
While the potential benefits are substantial, the FDA's decision has not been without controversy. There are ethical concerns surrounding xenotransplantation, particularly regarding animal welfare and the long-term consequences of modifying pig organs for human use. The FDA emphasizes the importance of conducting trials that are not only scientifically sound but also ethically responsible.
The approval of these studies also reflects broader shifts in medical research, as the quest for alternative solutions to organ shortages gains momentum. As the medical community watches closely, the outcomes of these studies could shape future policies and practices concerning organ transplantation for years to come.
In essence, the FDA's decision to allow human studies of pig kidney transplants is a groundbreaking step that holds the promise of life-saving treatments for countless patients. As the trials commence, the healthcare community remains hopeful that the lessons learned could usher in a new era of transplantation.
#Xenotransplantation #FDA #KidneyTransplant #OrganDonation #MedicalResearch #HealthcareInnovations #AnimalEthics
Author: Samuel Brooks




